Talk to your doctor. Learn what to expect before, during, and after surgery. Your questions may include:
In addition, do not hesitate to voice concerns or speak up if you do not understand something about your treatment
Getting in the best physical shape possible before surgery can lessen the chance for complications and shorten your recovery time.
Ask your doctor about exercises you can do before surgery. If you are having a hip or knee replacement, strengthening your upper body will make it easier to use crutches or a walker after surgery. Isometric exercises can help maintain the strength of your leg muscles. In addition, ask about the exercises that will be prescribed after surgery. If you become familiar with the exercises now, you will be ready to perform them after surgery. The 24 hours before your surgery will be a busy time filled with lots of last-minute preparations. Use this checklist to make sure that you do not forget anything:
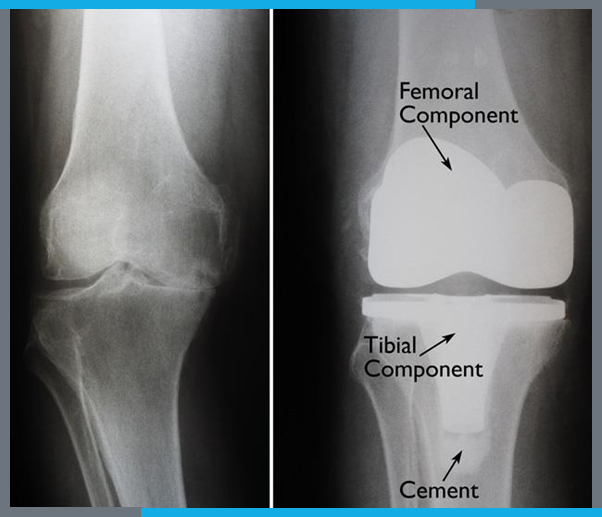
The surgical procedure usually takes from 1 to 2 hours. Your orthopaedic surgeon will remove the damaged cartilage and bone, and then position the new metal and plastic implants to restore the alignment and function of your knee.

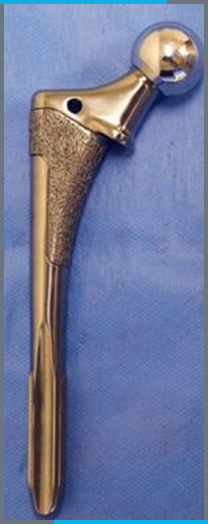
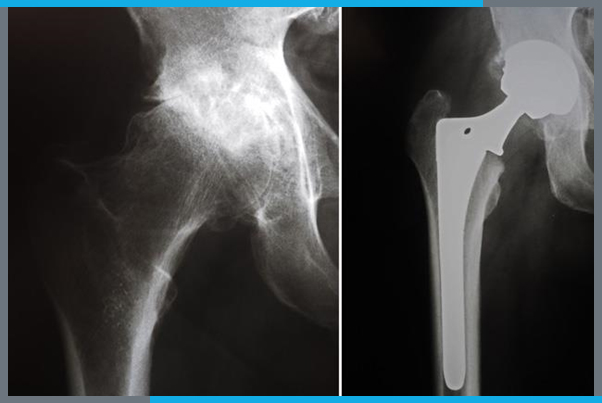
Many different types of designs and materials are currently used in artificial hip joints. All of them consist of two basic components: the ball component (made of highly polished strong metal or ceramic material) and the socket component (a durable cup of plastic, ceramic, or metal, which may have an outer metal shell).
The prosthetic components may be "press fit" into the bone to allow your bone to grow onto the components or they may be cemented into place. The decision to press fit or to cement the components is based on several factors, such as the quality and strength of your bone. A combination of a cemented stem and a non-cemented socket may also be used.
Your orthopaedic surgeon will choose the type of prosthesis that best meets your needs. The surgical procedure usually takes from 1 to 2 hours. Your orthopaedic surgeon will remove the damaged cartilage and bone and then position new metal, plastic, or ceramic implants to restore the alignment and function of your hip.

There are different types of shoulder replacements. Your surgeon will evaluate your situation carefully before making any decisions. They will discuss with you which type of replacement will best meet your health needs. Do not hesitate to ask which type of implant will be used in your situation, and why that choice is right for you.
The standard total shoulder replacement involves replacing the arthritic joint surfaces with a highly polished metal ball attached to a stem, and a plastic socket.
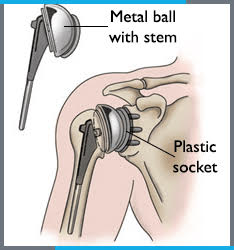
These components come in various sizes. They may be either cemented or press fit into the bone. If the bone is of good quality, your surgeon may choose to use a non-cemented (press-fit) humeral component. If the bone is soft, the humeral component may be implanted with bone cement. In most cases, an all-plastic glenoid (socket) component is implanted with bone cement.
Implantation of a glenoid component is not advised if:
Patients with bone-on-bone osteoarthritis and intact rotator cuff tendons are generally good candidates for conventional total shoulder replacement.
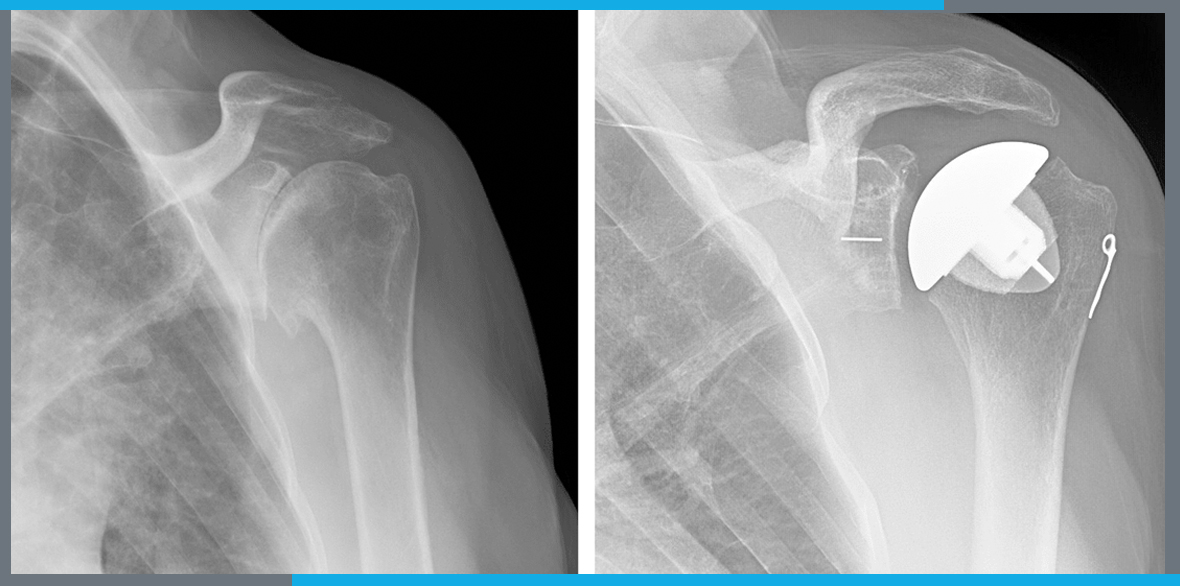
These X-rays were taken before and after total shoulder replacement surgery for osteoarthritis. Second X-ray shows the cap-like prosthesis used in resurfacing hemiarthroplasty.
Depending on the condition of your shoulder, your surgeon may replace only the ball. This procedure is called a hemiarthroplasty. In a traditional hemiarthroplasty, the surgeon replaces the head of the humerus with a metal ball and stem, similar to the component used in a total shoulder replacement. This is called a stemmed hemiarthroplasty.
Some surgeons recommend hemiarthroplasty when the humeral head is severely fractured but the socket is normal. Other indications for a hemiarthroplasty include:
Studies show that patients with osteoarthritis get better pain relief from total shoulder arthroplasty than from hemiarthroplasty.
Resurfacing hemiarthroplasty involves replacing just the joint surface of the humeral head with a cap-like prosthesis without a stem. With its bone-preserving advantage, it offers those with arthritis of the shoulder an alternative to the standard stemmed shoulder replacement.
Resurfacing hemiarthroplasty may be an option for you if:
For patients who are young or very active, resurfacing hemiarthroplasty avoids the risks of component wear and loosening that may occur with conventional total shoulder replacements in this patient population. Due to its more conservative nature, resurfacing hemiarthroplasty may be easier to convert to total shoulder replacement, if necessary, at a later time.
Another type of shoulder replacement is called reverse total shoulder replacement. Reverse total shoulder replacement is used for people who have:
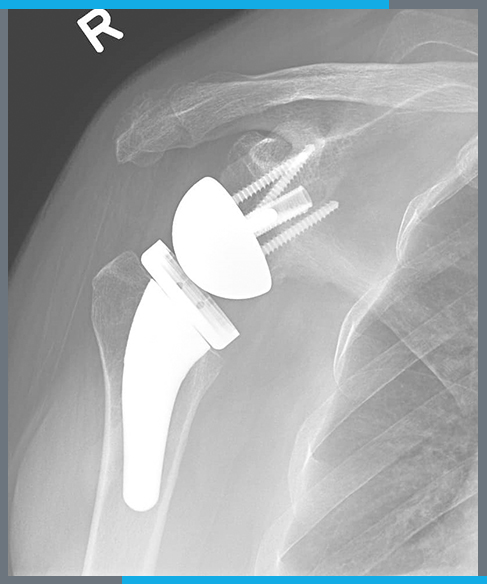
An X-ray of a reverse total shoulder replacement.
For these individuals, a conventional total shoulder replacement can still leave them with pain. They may also be unable to lift their arm up past a 90-degree angle. Not being able to lift your arm away from the side can be severely debilitating.
In reverse total shoulder replacement, the socket and metal ball are switched: A metal ball is attached to the shoulder bone, and a plastic socket is attached to the upper arm bone. This allows the patient to use the deltoid muscle instead of the torn rotator cuff to lift the arm.
To reach the elbow joint, your surgeon will make an incision (cut), usually at the back of the elbow. After making the incision, your surgeon will gently move muscles aside to access to bone. After removing scar tissue and spurs around the joint, your surgeon will prepare the humerus to fit the metallic piece that will replace that side of the joint. The same preparation is done for the ulna.
The replacement stems are placed into the humerus and ulna bones and kept in place with a bone cement. The two stems are connected by a hinge pin. Some newer types of elbow replacements are held together without a hinge and use the patient's own ligaments. These "non-linked" elbow replacements are not for everone; only certain patients without ligament injuries can have these types of implants.
After the wound is closed, a padded dressing is placed over the incision to protect it while it heals. Some surgeons will place a temporary small tube in the joint to drain the surgical fluid. This tube can be easily removed within the first few days after surgery.

An X-ray of a total elbow replacement taken from the side.
The metal replacement parts are made of chrome-cobalt alloy or titanium, and there is a liner made of polyethylene (plastic). The bone cement is made of polymethylmethacrylate (acrylic, a type of plastic)